In terms of rites of passage, perimenopause gets short shrift. For many women, it’s an uncomfortable in-between. They’ve aged out of their reproductive years but haven’t quite landed into “official” menopause. But instead of ignoring perimenopause, why not learn everything you can about this phase of life? For starters, it can begin much earlier (think thirties) and last much longer than you might think.
Secondly, let’s clarify the difference between perimenopause and menopause. Menopause is a point in time—the anniversary of your last menstrual period. Perimenopause (peri, Greek for "around" or "near" + menopause) is a much looser transitional state and can last anywhere from a few months to over a decade. The average length is four years.
Each woman experiences perimenopause differently. Some women have virtually no perimenopause symptoms, other women have a constant barrage of them. Hormones run amok or stay surprisingly stable. Periods may end abruptly or occur erratically; you may never get a single hot flash or experience multiple ones a day for years.
And several studies suggest that the earlier in perimenopause you start getting hot flashes, the longer they are likely to continue. An article published in Harvard Women's Health Watch, says “In numerical terms, women who started getting hot flashes when they were still having regular periods or were in early perimenopause experienced symptoms for a median of 11.8 years, nearly three times the median of 3.4 years for women whose hot flashes did not start until their periods stopped.”
If you suspect you are in perimenopause, there’s a lot you can do to ameliorate your symptoms. Here’s what to be on the lookout for.
Hot flashes and night sweats: Roughly half of perimenopausal women suffer sudden waves of body heat that last 5 to 10 minutes, that come on at night as well as during the day. Hot flashes tend to originate at the scalp, face, neck or chest. Women experience them with varying intensity that ranges from the slightly warm to the wringing wet.
What you can do: Avoid possible triggers of hot flashes, the most common of which include warm air temperatures, hot beverages and spicy foods. Another good idea is to dress in layers so you can take off clothes as needed.
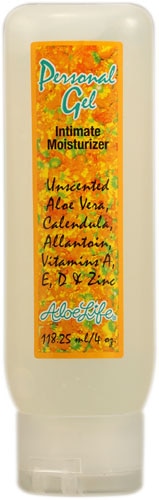
Vaginal dryness: As perimenopause progresses, falling estrogen levels can cause vaginal tissue to become thinner and drier. Vaginal dryness can cause itching, irritation and make intercourse painful.
What you can do: Many women get prescribed low-dose contraceptives or vaginal estrogen (in a cream, ring, tablet or gel) to help relieve vaginal dryness. You can also buy vaginal moisturizers such as Replens (available at drugstores and supermarkets), designed to increase vaginal moisture, elasticity and acidity. Continued sexual activity also seems to improve vaginal tone and alleviate dryness—just make sure you are fully aroused and relaxed before penetration occurs.
Sleep disturbances: According to the National Sleep foundation, approximately 61 percent of menopausal women have sleep problems. Some studies have shown a relationship between night sweats and disrupted sleep; others have not. And you can’t blame everything on hormones—sleep cycles change as we age, and both sexes tend to complain about insomnia.
What you can do: Good sleep hygiene is helped by keeping your bedroom reasonably cool and well-ventilated. Sheets and loose clothing made of natural fibers are best for sleeping. Avoid taking naps or excessive caffeine intake during the day, which will catch up to you at bedtime. Exercise and a regular bedtime schedule tend to make sleep deeper and longer.
Mood symptoms: Between roughly 10-20 percent of women experience mood symptoms during perimenopause. Some studies suggest there’s a link between decreasing estrogen and depression during the menopausal transition. But as of yet there’s no proof that declining hormone levels trigger depression in women at midlife. Interestingly, many studies show that women have a lower rate of depression after age 45 than before. Although the unpredictability of perimenopause can be stressful, the good news is that all the volatility will one day give way to a more even keel.
What you can do: The most telling predictors of mood symptoms at midlife are stress, poor overall health and a history of depression. Learning to manage stress better—through exercise, mindfulness, and meaningful work—can make a huge difference in how you experience the “change.”