If you’ve ever lied in bed at night with an uncontrollable urge to pee, a compulsion that you can’t renege on, you have had a minor bout of nocturia. Officially defined as waking up more than once during sleep to urinate, nocturia is an order of magnitude beyond the typical “well I’m up might as well pee” situation.

What is nocturia?
With nocturia, you literally have no choice but to get up and void your bladder. Getting up in the night, especially if it’s more than once, can cause sleep disruption, which in turn can impact quality of life. The more times a night you get up to void your bladder, the more severe the nocturia is considered.
If you have this problem, you’re not alone, nearly 1 in 3 adults over age 30 experience nocturia. It can be caused by underlying health issues or lifestyle habits and tends to increase with age.
When it comes to causes, there are a variety of reasons you may be experiencing nocturia.
Health issues that lead to nocturia (frequent urination at night)
Health issues include central nervous system disorders, which impair your ability to inhibit your urge to pee. Any condition, including sleep apnea, that impacts your brain function can impair your ability to control your bladder urges.
Cardiovascular disorders can also affect nocturia, because they cause the body to retain a great deal of fluid during the daytime. At night, the kidneys go into overdrive, producing a lot more urine, which leads to nocturia. The most common types of disease that cause this problem are congestive heart failure and severe varicose vein disease.
An overactive bladder often leads to a decreased capacity to hold urine and exacerbates the urge to void both day and night. Additionally, the bladder muscle can become disordered in many disease processes. Such conditions include diabetes, bladder cancer, cystitis, urinary tract infection, bladder stones, vaginal atrophy, pelvic prolapse, pelvic tumors, age-related atrophy of bladder muscle and enlarged prostate.
Certain medications can cause you to urinate more frequently, including diuretics, cardiac glycosides, demeclocycline, lithium, methoxyflurane, phenytoin, propoxyphene and excessive
vitamin D.
Lifestyle habits that can cause nocturia
- Drinking too much fluid, especially just before bedtime (especially caffeine or alcohol).
- Behavioral patterns such as training yourself to wake up during the night to use the bathroom, even if you don't necessarily have to go.
Ways to manage frequent urination at night
The first obvious thing you can do is check your fluid intake. The golden rule is to drink half your body weight in ounces each day, so if you weigh 120 pounds aim for 60 ounces of fluid per day. To ensure input and output is working correctly, monitor your fluid output. Your doctor can also provide you with a way to assess your urinary output.
If possible, time intake of
diuretics or other urination-inducing medications (take them mid- to late afternoon, six hours before bedtime).
If the amount of urine you produce isn’t too high, then you may have an issue with fully emptying your bladder. This can be due to bladder obstruction. Some women experience urinary retention due to bladder spasms, bladder inflammation and bladder pain (interstitial cystitis).
Assess for a health condition: Consult with your doctor to make sure you don’t have a urinary tract infection (symptoms include frequent and painful urination and occasionally blood in urine) and to rule out a metabolic disorder such as
diabetes.
Ask yourself: Have there been changes in your sleep patterns? If yes, consider getting an
Oura ring to track your sleep patterns. If your sleep has changed dramatically, see your doctor to find out why you might be experiencing these changes. Note some endocrine issues like hyperthyroidism (excess thyroid hormone) can be related to poor sleep.
If you are a female in your 30s and 40s, and you have increased urination at night consider seeing your gynecologist—you may have a fibroid that is pressing on your bladder causing you to have increased urge to urinate.
If you are in
menopause and experience some incontinence or leaking of a bit of urine when you cough or sneeze or jump, you may be having increased urination due to connective tissue changes in your vulva/vaginal/urethral area. The angle of the urethra changes when a woman’s estrogen levels drop due to changes in the architecture of the tissue—connective tissue break down—and the tissue thins and dries. See your gynecologist for possible hormonal solution such as vaginal estrogen.
Finally, particularly if you have had children, your pelvic floor may have become weakened. Post childbirth is a great time to start doing
Kegels to strengthen the pelvic floor and specifically the PC muscle (pubococcygeal muscle), the primary muscle that hold up the internal organs of the lower pelvis.
If all else fails, there are medications you can take to reduce the symptoms of an overactive bladder or assist the kidneys in producing less urine. Consult with your doctor about whether any of those prescriptions would be appropriate for you.
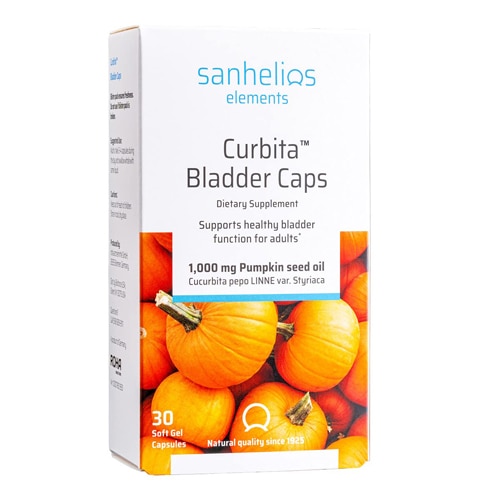
Featured products